The Journey to Healing: Understanding Complex Trauma Recovery
Complex trauma recovery is a step-by-step process that involves healing from repeated traumatic experiences. For women struggling with anxiety or betrayal trauma, or first responders dealing with occupational stress, understanding this recovery journey is essential. As a solo therapist at Brain Based Counseling, I offer specialized EMDR Intensive Therapy to help clients navigate this healing process in the Cincinnati area, including Indian Hill, Madeira, Mason, Hyde Park, Mount Lookout, Mount Adams, and Terrace Park, as well as virtual therapy for North Carolina residents.
Understanding Complex Trauma and Why It's Different
Complex trauma isn't simply a bad memory or a single frightening event. It's what happens when trauma becomes a repeated part of your daily life, especially when there's no clear way to escape it. The difference between complex trauma and single-incident trauma like a natural disaster is profound and requires a specialized approach to treatment.
Dr. Judith Herman, a Harvard psychiatrist who first coined the term "Complex PTSD" back in 1988, described it as repeated, chronic emotional pain or abuse, often suffered in childhood or adolescence. When trauma happens repeatedly, particularly during our formative years, it doesn't just create bad memories—it actually shapes how our brains develop and how our nervous systems function.
There's good news in the mental health field: the International Classification of Diseases (ICD-11) now officially recognizes Complex PTSD (C-PTSD) as its own distinct diagnosis, separate from traditional post-traumatic stress disorder (PTSD). This formal recognition validates what many survivors have felt all along—that their experiences and symptoms don't quite fit the standard PTSD model.
Core Symptoms You Might Notice
If you're on a complex trauma recovery journey, you might recognize some of these experiences:
Your emotions and feelings might feel overwhelming or unpredictable—like being on an emotional rollercoaster you can't get off. Many patients describe feeling either flooded by intense feelings or, alternatively, completely numb and disconnected. This emotional turmoil can make it challenging to cope with everyday situations.
You might struggle with a harsh inner critic and persistent feelings of shame. Unlike simple PTSD where the fear response is primary, complex trauma often leaves people feeling fundamentally flawed or unworthy. The shame that many survivors experience can be debilitating and affect how they form relationships.
Relationships can become particularly challenging. You might find yourself either avoiding close connections altogether or falling into patterns of relationships that somehow recreate aspects of past trauma. Many adults who experienced childhood trauma find that these relationship patterns persist well into adulthood.
Dissociation—those moments where you "check out" or feel detached from yourself—often serves as a protective mechanism that once helped you survive overwhelming experiences. Your body might remain on high alert, constantly scanning for danger (hypervigilance), or you might experience intrusive memories that feel as vivid as when they first occurred.
Many people also experience physical symptoms that don't have clear medical causes—chronic pain, digestive issues, or unexplained medical conditions. This mind-body connection is real and represents how trauma gets stored not just in our memories, but in our physical bodies.
Common Roots and Risk Factors
Complex trauma typically develops in situations involving power imbalances and repeated boundary violations. Some common causes include childhood trauma, physical abuse, emotional abuse, neglect, ongoing domestic violence, sex trafficking, human trafficking, prolonged exposure to war, refugee experiences, repeated medical trauma, chronic caregiver mistreatment, or other forms of experienced trauma.
The groundbreaking ACE (Adverse Childhood Experiences) Study has been instrumental in helping us understand these connections. According to research on ACEs, about 61% of adults surveyed across 25 U.S. states report experiencing at least one adverse childhood experience. More concerning, one in six reported experiencing four or more ACEs, which significantly increases health risks later in life.
It's important to acknowledge that trauma exposure isn't distributed equally across communities. Research shows that 61% of Black non-Hispanic children and 51% of Hispanic children in the U.S. have experienced at least one ACE, compared with 40% of white non-Hispanic children and 23% of Asian non-Hispanic children. These disparities highlight how social inequities and historical trauma can compound individual experiences.
When the brain is developing and repeatedly exposed to danger without adequate support, the amygdala (our brain's alarm system) becomes hypersensitive. This creates what therapists call "amygdala hijack"—where your threat-response system activates even in safe situations. Meanwhile, parts of the brain responsible for logical thinking and emotional regulation may not develop optimally, making it harder to process emotions or think clearly when triggered.
Understanding these neurobiological changes isn't about making excuses—it's about recognizing that complex trauma recovery requires approaches that address both psychological and physiological symptoms. Your struggles aren't a character flaw or weakness; they're normal responses to abnormal situations.
At Brain Based Counseling, I specialize in therapy approaches that address both the mind and body aspects of trauma, recognizing that true healing happens when we work with both your story and your nervous system. Every person's trauma is unique, which is why your recovery journey should be custom specifically to you.
The Roadmap to Complex Trauma Recovery
Recovery from complex trauma isn't a straight path—it's more like a gentle spiral where you revisit similar themes as you heal more deeply. While everyone's journey is unique, having a roadmap can provide much-needed structure and hope along the way.
It's important to be patient in the recovery process, as healing often occurs in relationships with others, such as family, friends, or peers. For many survivors, learning to feel safe in relationships again is a critical part of healing.
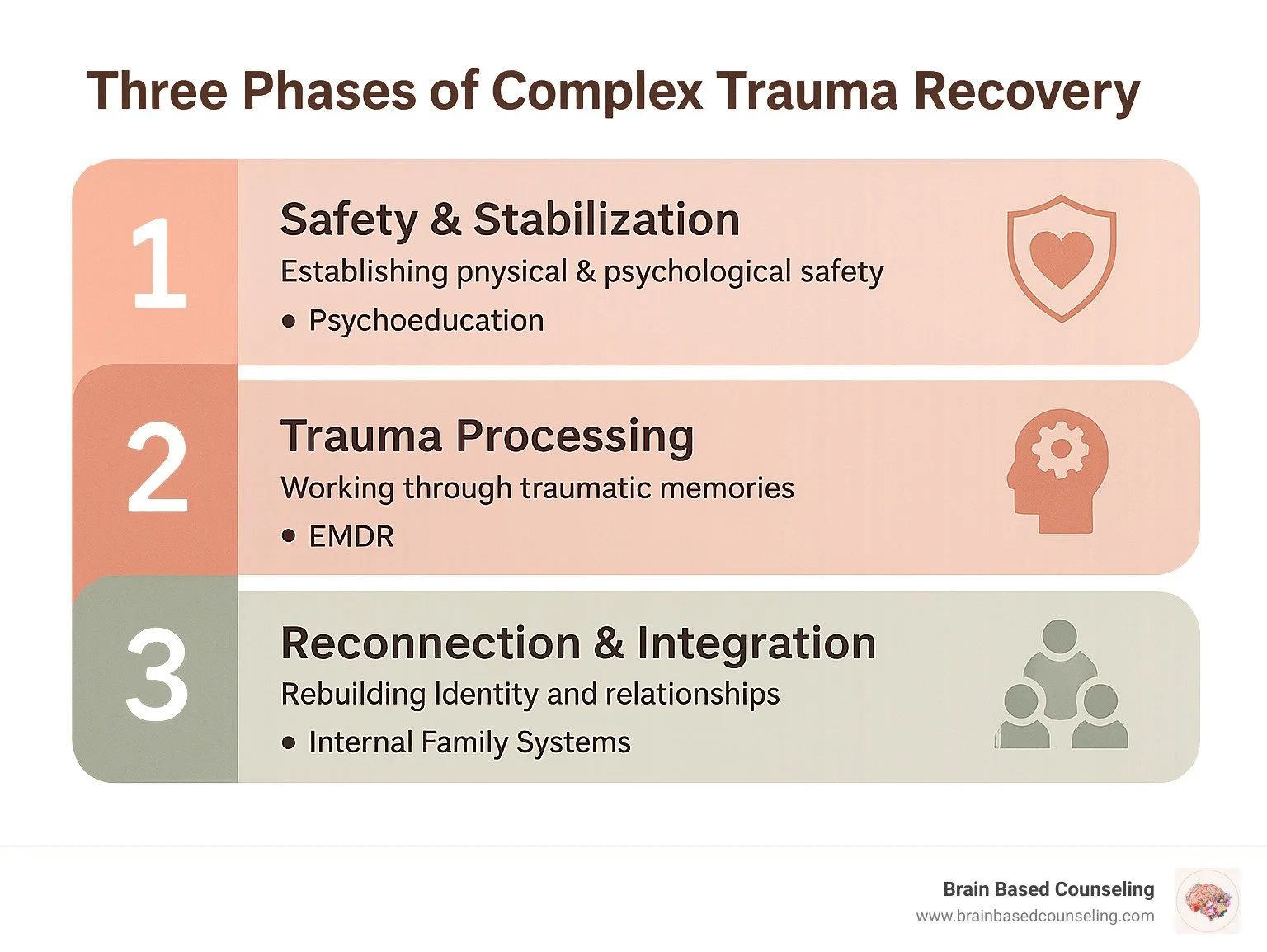
The most respected framework for complex trauma recovery comes from Dr. Judith Herman, who outlined three main phases that have since become the gold standard in trauma treatment:
Safety and Stabilization
Remembrance and Mourning
Reconnection and Integration
This phased approach isn't just theory—it's endorsed by trauma experts worldwide because it ensures you develop essential coping skills before diving into painful memories. As renowned trauma specialist Bessel van der Kolk beautifully puts it in "The Body Keeps the Score": "Recovery from trauma involves (re)learning how to be calm, alive, and engaged."
I want to reassure you that these stages aren't rigid boxes—you'll likely move back and forth between them as needed. Some days you might need to focus on stabilization techniques, while on others you might feel ready to process memories or work on rebuilding connections. This natural ebb and flow is completely normal and expected.
Stage 1: Creating Safety & Stabilization
The foundation of all trauma healing begins with establishing safety—both physical and emotional. Without this crucial groundwork, attempting to process traumatic memories can feel overwhelming and sometimes even make symptoms worse. Feeling safe is essential for individuals recovering from complex PTSD (C-PTSD), as it helps them build trust and a sense of security in their relationships.
During this first phase, we'll focus on building your inner resources and outer support systems. This includes learning grounding techniques that help you stay present when memories or emotions feel intense. We'll work on emotional regulation skills—simple but powerful ways to calm your nervous system when it gets activated.
Establishing external safety is equally important. This might mean creating healthier boundaries in relationships or making changes to your environment that help you feel more secure. We'll also look at stabilizing daily functioning through improved sleep habits, nutrition, and basic self-care—all of which directly impact your ability to heal.
Understanding how trauma affects your brain and body can be incredibly empowering. Many people find that simply learning about their trauma responses helps them feel more validated and in control. For example, learning about how the brain processes fear and stress can help normalize your experiences and reduce shame.
This stage often takes time—sometimes months—and that's completely normal. I've found in my work at Brain Based Counseling that rushing through stabilization often backfires. As we say in trauma therapy: "Go slow to go fast."
Stage 2: Processing Memories Without Overwhelm
Once you've established a solid foundation of safety and stabilization skills, we can begin to process traumatic memories. This doesn't mean reliving the trauma—instead, it means working through memories in a way that helps your brain process them without becoming overwhelmed.
The key to this stage is what therapists call "titrated exposure"—approaching traumatic memories gradually, at a pace that feels manageable for you. We'll practice maintaining "dual awareness," keeping one foot in the present (where you're safe) while exploring past experiences.
What's happening neurologically during this phase is fascinating: your brain is actually reconsolidating memories, storing them in a way that reduces their emotional charge. This memory processing helps alleviate the emotional impacts of trauma, making the memories "just something that happened" rather than something that continues to intrude on your daily life.
EMDR therapy (Eye Movement Desensitization and Reprocessing) shines particularly bright during this stage because it helps the brain process traumatic memories without requiring detailed verbal recounting of every painful moment. This makes it especially valuable for complex trauma recovery where there may be multiple traumatic memories or trauma that occurred before you had the words to describe it.
As trauma expert Dr. Peter Levine wisely notes: "Trauma is not what happens to us, but what we hold inside in the absence of an empathetic witness." This stage provides that compassionate witnessing in a safe, controlled environment.
Stage 3: Reconnection, Identity, and Meaning
The final stage of complex trauma recovery focuses on reconnecting with yourself, others, and the world around you. This is where many survivors experience profound growth and change.
During this phase, we'll explore who you are beyond your trauma. Many survivors have had their person's identity shaped by traumatic experiences, and finding who you truly are can be both challenging and deeply rewarding. We'll work on building healthy relationships, often applying new boundaries and communication skills learned earlier in treatment.
Finding meaning in your experiences becomes possible at this stage. While this doesn't mean the trauma "happened for a reason," many survivors find ways to integrate their experiences into a coherent life narrative that acknowledges both pain and resilience.
Looking toward the future becomes easier now. Setting goals and pursuing dreams that trauma may have interrupted is a powerful part of reclaiming your life. Many clients experience what psychologists call "post-traumatic growth"—recognizing the strengths, wisdom, and compassion they've developed through their healing journey.
As trauma specialist Dr. Janina Fisher notes: "Recovery isn't just about addressing symptoms—it's about reclaiming your life and sense of self."
Some survivors find that giving back to others or engaging in advocacy work becomes meaningful during this stage. As one survivor shared: "Using my experience to help others gave meaning to what I went through. It didn't erase the pain, but it transformed it into something purposeful."
Throughout your complex trauma recovery journey at Brain Based Counseling, I'll be there to guide, support, and witness your progress through each of these stages. The path isn't always easy, but with the right support and tools, healing is absolutely possible—and the freedom waiting on the other side is worth every step.
Evidence-Based Therapies and Brain-Body Modalities for Complex PTSD
When it comes to complex trauma recovery, not all therapeutic approaches deliver the same results. The research is clear: treatments that address both the mind and body aspects of trauma work best. This makes perfect sense when you think about it—trauma isn't just stored in our memories; it lives in our bodies too. Complex trauma can manifest in various forms of emotional, physical, and mental distress, and addressing these various aspects requires a multifaceted approach.
EMDR (Eye Movement Desensitization and Reprocessing) stands out as particularly effective for complex trauma and to treat PTSD. Unlike traditional talk therapy where you might spend years discussing painful experiences, EMDR helps your brain process traumatic memories through bilateral stimulation—essentially helping your brain "unstick" from trauma.
At Brain Based Counseling, I specialize in EMDR therapy, particularly through intensive formats that can accelerate healing for women dealing with complex trauma. This concentrated approach can help you make significant progress in a shorter timeframe than traditional weekly sessions might allow.
Why EMDR Excels in Complex Trauma Recovery
EMDR has gained substantial recognition for good reason. What makes it particularly suited for complex trauma recovery is how it works with your brain's natural healing processes.
When we experience trauma, especially repeated trauma, our brains can't process the experiences normally. The memories get stored with all the original emotions, beliefs, and physical sensations intact. EMDR helps your brain reprocess these memories so they become less emotionally charged and more integrated into your life story.
What I love about EMDR for my clients is that you don't need to describe traumatic experiences in excruciating detail. This can be such a relief, especially for those with preverbal trauma or experiences that feel impossible to put into words. Many people appreciate that with EMDR, they can process their experiences without having to narrate every painful detail.
The results tend to be both profound and lasting. Your brain actually changes how it stores the memories, which is why the improvements typically stick around long after treatment ends. This isn't just my clinical observation—the American Psychological Association, World Health Organization, and U.S. Department of Veterans Affairs all recognize EMDR as effective for trauma treatment.
Creating a sense of safety and stability is vital in the recovery process from complex PTSD (C-PTSD). It lays the foundation for addressing deeper traumatic memories and behaviors. Treatment focuses on both the neurobiological and psychological aspects of trauma.
EMDR intensives—which I offer at Brain Based Counseling—can be particularly powerful for complex trauma. These condensed, focused treatment periods compress months of weekly therapy into a concentrated timeframe, allowing for deeper processing and potentially faster symptom relief.
Complementary Approaches That Boost Results
While EMDR provides a powerful foundation for healing complex trauma, I've found that integrating complementary approaches creates a more comprehensive path to recovery. Think of it like building a house—EMDR may be the frame, but these additional approaches add important finishing elements. Chronic trauma, often referred to as long term trauma, can lead to complex post-traumatic stress disorder (C-PTSD), affecting emotional processing and relationships. Addressing these enduring stressors requires a multifaceted approach.
Polyvagal-informed interventions have been game-changers for my clients. Based on Dr. Stephen Porges' groundbreaking work, these techniques help regulate your nervous system, teaching it to feel safe again. These techniques can help find relief from the constant fight-or-flight response that many trauma survivors experience.
HeartMath practices offer evidence-based tools that improve the communication between your heart and brain, enhancing emotional regulation. These simple but powerful techniques can help manage the emotional overwhelm that often comes with complex trauma.
Mindfulness techniques build present-moment awareness and reduce reactivity—crucial skills when trauma responses frequently pull you into the past. Mindfulness can serve as an anchor to the present when flashbacks and traumatic memories pull you toward the past.
Body-based approaches address trauma stored in the physical body. As trauma expert Dr. Bessel van der Kolk famously wrote, "The body keeps the score." Many of my clients find that physical sensations hold important keys to their healing.
Self-compassion work helps counter the harsh self-criticism that often accompanies complex trauma. Learning to treat yourself with the same kindness you'd offer a good friend can be transformational when trauma has taught you that you don't deserve gentleness.
The beauty of these complementary approaches is that they're not just for our therapy sessions—they become tools you can use independently in your daily life. Many clients tell me that learning these skills has been as valuable as the trauma processing itself, giving them confidence that they can manage difficult moments on their own.
Complex trauma recovery isn't just about addressing symptoms—it's about reclaiming your life and rebuilding your relationship with yourself. The right therapeutic approach can make all the difference in this journey.
Everyday Resilience: Coping Strategies & Lifestyle Shifts
Living with the effects of complex trauma doesn't end when you leave your therapy session. Complex trauma recovery is a journey that weaves through every aspect of your daily life. The good news? Small, consistent practices can create powerful shifts in your healing process over time.
For example, starting your day with a grounding ritual, such as the 5-4-3-2-1 sensory exercise, can help manage daily stress and stay present.
I've seen this with my clients at Brain Based Counseling. The women who build resilience-boosting habits into their everyday routines often make the most profound progress. These aren't complicated techniques—they're simple practices that, when done consistently, help rewire the brain and nervous system toward safety and connection.
Think of these strategies as daily supplements to your therapy work—they reinforce the healing that happens in our sessions together and help you build your own internal resources for managing triggers and stress.
Grounding rituals can be particularly powerful. Something as simple as taking five minutes each morning to practice the 5-4-3-2-1 sensory exercise—noticing five things you can see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste—can anchor you in the present moment when trauma responses want to pull you into the past.
Quality sleep is another cornerstone of trauma healing that often gets overlooked. When we sleep, our brains process emotional experiences and consolidate learning. Creating a consistent sleep routine, limiting screen time before bed, and making your bedroom a sanctuary can dramatically impact your recovery journey.
Movement deserves special attention in complex trauma recovery. Trauma gets stored in the body, and gentle, mindful movement helps release that stored tension. This doesn't mean forcing yourself into high-intensity workouts—a mindful walk, gentle stretching, or trauma-sensitive yoga can be incredibly effective. The key is finding movement that feels good and safe in your body.
Mindfulness practices create space between your thoughts and reactions, giving you more choice in how you respond to triggers. Even just three minutes of mindful breathing can activate your parasympathetic nervous system and bring you back to a state where you can think clearly rather than react from trauma.
Creative expression offers a pathway to process emotions that might be difficult to put into words. Many of my clients find that journaling, drawing, dancing, or playing music helps them connect with and release feelings that have been stuck for years. Creative activities like watercolor painting can allow for expression of grief that might be difficult to verbalize, giving voice to parts of yourself that have been silenced.
Nature connection provides a gentle but powerful reset for an overwhelmed nervous system. Research shows that even 20 minutes in a natural setting can lower stress hormones and promote a sense of wellbeing. The predictable rhythms of nature can be especially soothing for a system that's been shaped by unpredictable trauma.
Building supportive relationships might be the most healing element of all. Trauma often happens in relationship, and healthy relationships are essential for healing. This doesn't mean you need a large social circle—even one or two safe, consistent connections can make a tremendous difference in your recovery journey.
Helpful vs. Unhelpful Coping
Not all ways of managing difficult emotions support healing. In fact, some of the strategies that might have helped you survive trauma can actually keep you stuck if relied on long-term.
When we're overwhelmed, it's natural to reach for whatever brings immediate relief. Substance use often starts this way—alcohol or other substances can temporarily quiet the noise of trauma symptoms. But over time, they can prevent the processing needed for true healing and create additional problems.
Overworking is another common coping strategy I see among high-functioning women with trauma. Keeping constantly busy can be an effective way to avoid painful feelings, but it also prevents the integration needed for healing. This pattern can feel like running on a hamster wheel to stay one step ahead of difficult feelings.
People-pleasing behaviors often develop as survival strategies during trauma, especially childhood trauma. While being attuned to others' needs isn't inherently problematic, consistently prioritizing others at your own expense reinforces the trauma-based belief that your needs don't matter.
The path to healing isn't about harshly judging these coping mechanisms—they helped you survive. Instead, it's about gently recognizing when they're no longer serving you and developing alternatives that support your wellbeing. Many people find it helpful to acknowledge how these patterns once protected them while recognizing when it's time to develop healthier coping strategies.
Healthier alternatives might include reaching out to a support person when emotions feel overwhelming, practicing grounding techniques when triggered, or engaging in physical activity to release tension. The goal isn't perfect coping but developing a wider range of options for managing difficult moments.
While short-term trauma from a natural disaster can lead to immediate psychological effects, it is distinct from the long-term impacts of complex trauma, which arises from repeated or prolonged traumatic experiences.
Building a Personalized Safety Plan
One of the most valuable tools I create with clients during complex trauma recovery is a personalized safety plan. This isn't a generic handout but a carefully crafted resource custom to your specific triggers, warning signs, and effective coping strategies.
A good safety plan starts with identifying your personal triggers—the situations, sensations, or interactions that activate your trauma responses. These might include certain locations, anniversary dates, specific phrases, or even sensory experiences like particular smells or sounds.
Next, we map your early warning signs—the subtle physical and emotional signals that indicate you're beginning to get triggered. These might include tension in specific parts of your body, changes in breathing, racing thoughts, or emotional shifts. Recognizing these early signs gives you a chance to respond before you're in full fight-flight-freeze mode.
The heart of the safety plan is your personalized toolkit of regulation strategies—specific practices that help you return to a state of relative calm. For some clients, this includes sensory grounding techniques like holding an ice cube or smelling essential oils. For others, movement practices like gentle stretching or progressive muscle relaxation work best.
Your safety plan should also include social resources—specific people you can reach out to when you're struggling. This might include friends, family members, your therapist, or support groups. Having these contacts readily available prevents the isolation that often accompanies trauma responses.
Finally, every safety plan should include professional resources for moments of crisis—your therapist's contact information, crisis text lines, and local emergency services. While you may never need these resources, having them readily available can provide peace of mind.
At Brain Based Counseling, I work with each client to develop and refine this personalized plan throughout our work together. We test what works, adjust what doesn't, and create a living document that evolves as you progress in your recovery journey. This concrete tool provides a roadmap for navigating difficult moments and reinforces that you're never alone in this process.
Building resilience isn't about never struggling—it's about having effective tools to help you return to balance when you do. With consistent practice and compassionate support, these everyday strategies can transform your relationship with trauma and open the door to a life defined by possibility rather than pain.
Accessing Support and Moving Forward
Taking that first step to reach out for professional help is often both the hardest and most important part of your complex trauma recovery journey. I know that finding the right support can sometimes feel overwhelming, especially when you're already managing the daily challenges of trauma symptoms.
When searching for a trauma therapist, there are several key factors worth considering that can make all the difference in your healing experience:
First, look for a professional with specific training in complex trauma. Not all therapists have specialized training in trauma-informed care, and complex trauma requires an even more nuanced understanding than single-incident trauma. A specialist will recognize the unique patterns and needs that come with developmental or repeated trauma.
The therapeutic approach matters too. Some modalities like EMDR, Somatic Experiencing, and trauma-focused CBT have stronger evidence for trauma healing than generalized talk therapy. Consider whether their methods align with what feels right for you.
Perhaps most importantly, trust your instincts about the connection. Research consistently shows that the therapeutic relationship itself is one of the strongest predictors of successful outcomes in therapy. You deserve to work with someone who feels safe, understanding, and genuinely attuned to your needs.
Practical considerations matter too—location, telehealth options, session frequency, and financial arrangements all play a role in whether therapy will be sustainable for you long-term.
At Brain Based Counseling, I specialize in helping women with high-functioning anxiety and complex trauma through EMDR therapy. I offer both in-person sessions in the Cincinnati area, including Indian Hill, Madeira, Mason, Hyde Park, Mount Lookout, Mount Adams, and Terrace Park, and virtual sessions throughout Ohio and North Carolina, making healing accessible whether you prefer face-to-face connection or the comfort of your own space.
Frequently Asked Questions about Complex Trauma Recovery
I find that many clients come to me with similar questions about what to expect from the healing journey. Here are thoughtful answers to some of the most common questions:
How long does complex trauma recovery take?
This is perhaps the question I hear most often, and I wish I could offer a simple timeline. The truth is that recovery varies significantly based on many factors: the severity and duration of trauma, how early in life it occurred, what support systems you have in place, and your individual resilience factors.
While some people experience meaningful symptom relief within months, complex trauma recovery is typically measured in years rather than weeks or months. This isn't meant to discourage you—many clients notice significant improvements in specific symptoms quite quickly, particularly with approaches like EMDR. Rather, healing tends to unfold in layers, with each layer bringing new insights and growth.
As trauma expert Judith Herman wisely notes: "The resolution of trauma is never final; recovery is never complete. The impact of a traumatic event continues to reverberate throughout the survivor's lifecycle." This doesn't mean you'll always struggle intensely, but rather that healing becomes an integrated part of your life journey.
Can EMDR therapy be done virtually?
Yes! Research increasingly shows that EMDR therapy can be effectively delivered through telehealth platforms. At Brain Based Counseling, I offer virtual EMDR sessions for clients throughout Ohio and North Carolina using secure, HIPAA-compliant video platforms.
For online EMDR, we use various adaptations for the bilateral stimulation component—from visual tracking on your screen to self-administered bilateral tapping. Many clients actually prefer virtual EMDR once they try it, appreciating the comfort of processing difficult memories in their own safe space rather than having to drive home afterward.
Is full recovery from complex trauma possible?
Yes, significant healing and recovery from complex trauma are absolutely possible. I've witnessed this change countless times in my practice, and research supports it too. While the goal isn't to erase your past—those experiences will always be part of your story—you can reach a place where trauma no longer controls your daily life, relationships, or sense of self.
Many survivors achieve symptom resolution, develop healthier relationships, experience greater joy and presence, and even find what psychologists call post-traumatic growth—finding new meaning, strength, and wisdom through their healing journey.
With time and proper treatment, many people reach a point where they're no longer defined by what happened to them. The trauma becomes part of their story but no longer the whole story.
Finding the Right Help for You
Finding a therapist who truly understands complex trauma and creates a safe space for healing is crucial. When searching for the right fit, consider asking potential therapists these questions:
"What specialized training do you have in trauma treatment?" Look for specific certifications or extensive training in evidence-based trauma approaches, not just general counseling experience.
"What specific approaches do you use for complex trauma?" Their answer should demonstrate knowledge of phased treatment and trauma-specific modalities like EMDR, Somatic Experiencing, or other evidence-based methods.
"How do you ensure safety and stabilization before processing trauma?" A knowledgeable trauma therapist will emphasize the importance of building coping skills before diving into trauma processing.
"How do you help clients manage overwhelming emotions?" Their response should include specific strategies for emotional regulation and grounding.
"What is your experience with my specific type of trauma?" While therapists don't need personal experience with your trauma type, they should have professional experience and understanding of the particular challenges it presents.
At Brain Based Counseling, I offer a free 15-minute consultation to help determine if my approach aligns with your needs. This gives you the opportunity to ask questions and get a sense of whether we might work well together before committing to therapy. It's like a brief introduction where we both get to see if we're a good match for this important work.
I can provide documentation for out-of-network benefits for those with PPO insurance plans. Many clients find that the focused, efficient nature of EMDR intensive therapy ultimately provides good value compared to years of weekly therapy sessions, though I invite you to reach out directly to discuss the investment and what might work best for your situation.
Finding the right therapist sometimes takes time, and it's okay to meet with several before deciding. This relationship is too important to settle—you deserve someone who gets you, respects you, and has the skills to help you heal.
The journey through complex trauma recovery isn't easy, but you don't have to walk it alone. With the right support, healing is not just possible—it's happening for survivors every day. Your healing journey can begin whenever you're ready to take that first step.
Conclusion
Complex trauma recovery is challenging but absolutely possible. The journey from pain to peace requires courage, support, and effective therapeutic approaches that address both the psychological and physiological impacts of trauma.
At Brain Based Counseling, I specialize in helping women with high-functioning anxiety and complex trauma through EMDR therapy. My brain-based approach addresses the root causes of trauma symptoms, not just the surface manifestations, leading to more complete and lasting healing.
Whether you're just beginning to recognize the impact of past trauma or you've been on your healing journey for some time, know that additional support and relief are available. EMDR intensives offer an accelerated path to processing traumatic memories and reducing symptoms, often accomplishing in days what might take months in weekly therapy.
As trauma expert Dr. Bessel van der Kolk reminds us: "The greatest sources of our suffering are the lies we tell ourselves." One of those lies is that we can't heal from complex trauma—but research and countless survivor stories prove otherwise.
Your past experiences have shaped you, but they don't have to define your future. With the right support and therapeutic approaches, you can move from simply surviving to genuinely thriving.
If you're ready to take the next step in your healing journey, I invite you to reach out for a free 15-minute consultation. Together, we can discuss your unique situation and determine if my approach at Brain Based Counseling might be the right fit for your complex trauma recovery needs.
Remember: healing is not linear, and it takes time—but with each step forward, you reclaim more of yourself and your life. The path from pain to peace is possible, and you don't have to walk it alone.